The Centre released an advisory for screening, diagnosis and management of mucormycosis or ‘black fungus’ that is being widely reported among COVID-19 survivors
The Central government on Sunday released an advisory for screening, diagnosis and management of mucormycosis or ‘black fungus’ infection that is being widely reported among COVID-19 survivors in the country. According to the Union Health Ministry, mucormycosis is a fungal infection that mainly affects people who are on medication and reduces their ability to fight environmental pathogens. Sinuses or lungs of such individuals get affected after fungal spores are inhaled from air and it may turn fatal if not cared for.
The Health Ministry and ICMR that have been in the frontline of the government’s battle against the pandemic have prepared guidelines to prevent or manage the disease.
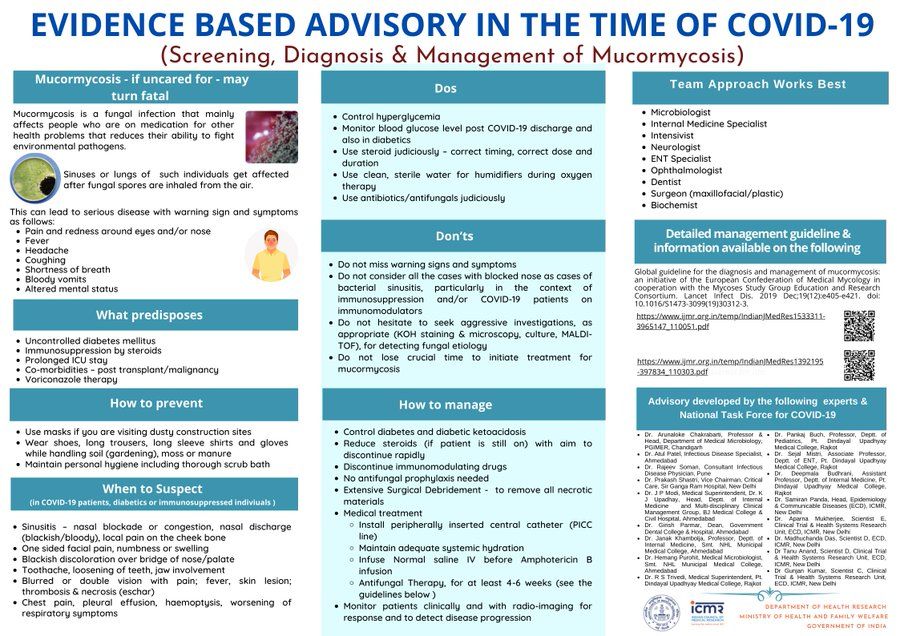
Sign and symptoms of mucormycosis/black fungus
- Pain and redness around eyes and/or nose
- Fever
- Headache
- Coughing
- Shortness of breath
- Bloody vomits
- Altered mental status
What are the predispositions
- Uncontrolled diabetes mellitus
- Immunosuppression by steroids
- Prolonged ICU stays
- Co-morbidities – post-transplant/malignancy
- Voriconazole therapy
What should you do?
- Control hyperglycemia
- Monitor blood glucose level after COVID-19 recovery and also in diabetics
- Use steroid judiciously – correct timing, correct dose and duration
- Use clean, sterile water for humidifiers during oxygen therapy
- Use antibiotics/antifungals judiciously
What should you not do?
- Do not miss warning signs and symptoms
- Do not consider all the cases with a blocked nose as cases of bacterial sinusitis, particularly in the context of immunosuppression and/or COVID-19 patients on immunomodulators
- Do not hesitate to seek aggressive investigations, as appropriate (KOH staining & microscopy, culture, MALDITOF), for detecting fungal aetiology
- Do not lose crucial time to initiate treatment for mucormycosis
How to prevent mucormycosis/black fungus?
- Use masks if you are visiting dusty construction sites
- Wear shoes, long trousers, long sleeve shirts and gloves while handling soil (gardening), moss or manure
- Maintain personal hygiene, including thorough scrub bath
When to suspect the fatal infection?
(in COVID-19 patients, diabetics or immunosuppressed individuals)
- Sinusitis – nasal blockage or congestion, nasal discharge (blackish/bloody), local pain on the cheekbone or one-sided facial pain, numbness or swelling
- Blackish discolouration over the bridge of nose/palate
- Toothache, loosening of teeth, jaw involvement
- Blurred or double vision with pain; fever, skin lesion; thrombosis & necrosis (eschar)
- Chest pain, pleural effusion, haemoptysis, worsening of respiratory symptoms
How to manage mucormycosis?
- Control diabetes and diabetic ketoacidosis
- Reduce steroids (if the patient is still on) with the aim to discontinue rapidly
- Discontinue immunomodulating drugs
- No antifungal prophylaxis needed
- Extensive Surgical Debridement – to remove all necrotic materials
- What is the medical treatment for mucormycosis?
- Install peripherally inserted central catheter (PICC line)
- Maintain adequate systemic hydration
- Infuse normal saline IV before Amphotericin B infusion
- Antifungal therapy, for at least 4-6 weeks (follow guidelines)
- Monitor patients clinically and with radio-imaging for response and to detect disease progression
Whom should you consult?
- Microbiologist
- Internal Medicine Specialist
- Intensivist Neurologist
- ENT Specialist
- Ophthalmologist
- Dentist Surgeon (maxillofacial/plastic)
- Biochemist